Newly Discovered Protein Complex in RAS Pathway May Provide a Treatment Target
In terms of cancer research, there’s a full-court press underway in collaborative scientific efforts targeting oncogenic RAS mutations. For decades, these mutations have been considered undruggable.
The RAS signaling pathway is extraordinarily complicated. It is also the most frequently mutated oncogene in human cancers. Approximately 30 percent of all human cancers are driven by mutations of the RAS family of genes. One member of this gene family is called KRAS, and it’s implicated in more than 90 percent of pancreatic malignancies. Cancers carrying a RAS mutation are typically highly aggressive and recurrent, sending signaling commands through the RAS pathway.
Now, in a study published in the journal Nature, scientists from Dana-Farber Cancer Institute (DFCI) and the Broad Institute of MIT and Harvard have determined the molecular structures of the RAS-pathway protein SHOC2 and two other proteins it binds. The three-protein SHOC2-MRAS-PP1C, or the so-called SMP complex, regulates the RAS signaling system and aids in the survival of cancer cells that have RAS mutations. This finding may provide the key to new targeted therapy drugs offering pancreatic cancer patients and others the chance for longer-term survival.
The study is “very exciting,” says gastrointestinal oncologist Allyson Ocean, M.D., of NewYork-Presbyterian/Weill Cornell Medical Center. “This is so promising because the RAS pathway is implicated not just in pancreatic cancer but in many other cancers like lung and colon cancer that affect millions of people in the world,” she explains. “There is even the potential with this finding to help with diseases outside of cancer, too.”
A Little Biochemistry Primer
When we are healthy, RAS signaling is central to the seamless functioning of cell signaling networks involved in cell growth and survival. Like many cellular signaling pathways, however, mutations can arise in cancer that lead the complex cascade of signaling to go very wrong. These mutations in the RAS gene itself, or in upstream or downstream regulators, can morph the normal cell proliferation, growth, and survival of cancer cells into dysregulated processes that lead to aggressive cancer.
The best way to think of the RAS pathway is like a kind of chain reaction. Although the pathway is complex and fraught with acronyms, it is pretty straightforward. RAS activates RAF; RAF activates MEK; MEK activates ERK; and ERK promotes irregular cell proliferation and tumor growth. But, unfortunately, what researchers have found is that blocking cancer cells at any single target in this pathway is generally not enough to halt the spread of cancer. That’s because a cancer cell turns on other nodes in the RAS pathway. Cancer can even activate parallel pathways in order to survive.
One such cancer drug aimed at a RAS pathway is called a MEK inhibitor. This drug blocks proteins called MEK1 and MEK2, which help control cell growth and survival. Blocking these proteins may help keep cancer cells from growing and may kill them.
“What Would Be the Best Targets?”
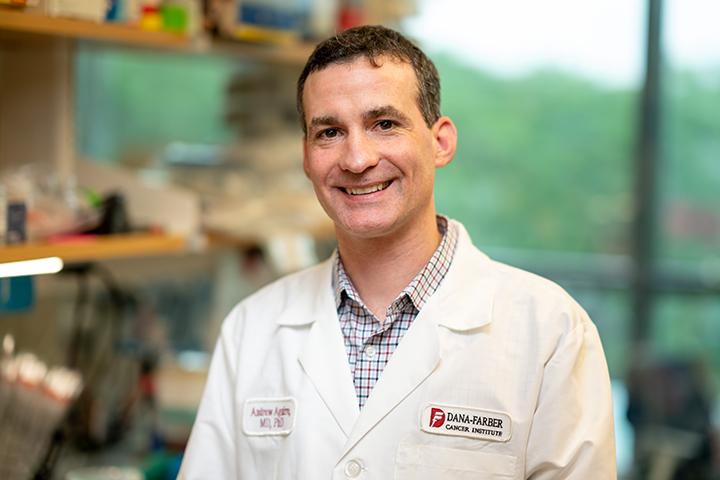
A few years ago, work in laboratories at DFCI and the Broad Institute led by physician–scientists Andrew Aguirre, M.D., Ph.D., and William Hahn, M.D., Ph.D., began looking at MEK1/2 inhibition in more detail. The team knew MEK inhibition was a promising strategy against pancreatic cancer. But tumors quickly acquired resistance to the drug that was tested, and there were significant toxicities associated with it.
“We asked the question of what would be the best targets to inhibit in combination with a MEK inhibitor to improve the efficacy of this therapy,” says Aguirre, co-senior author of the Nature study.
To discover the answer, the team conducted a series of unbiased genome-scale genetic screens to identify novel targets that enhance the effectiveness of MEK inhibition in KRAS mutant cancer cells. “To make a long story short, we identified that knocking out or depleting the SHOC2 gene disrupted survival pathways,” Aguirre explains. More studies showed that SHOC2 knockout in combination with MEK inhibitor treatment led to ablation of tumor growth in xenograft mice.
Further collaborative research led by Jason Kwon, Ph.D., Behnoush Hajian, Ph.D., and Yuemin Bian, Ph.D., in the laboratories of Aguirre, Hahn, and Christopher Lemke, Ph.D., at DFCI and the Broad Institute, revealed the structure of SHOC2 and the proteins it interacts with. “On its own, SHOC2 looked like a half-cylinder, solenoid-shaped structure that didn’t have any pockets,” says Aguirre. The team delved deeper and looked at two key proteins that SHOC2 brings together. The proteins are called MRAS and PP1C, and they are part of the RAS pathway. “The three-protein structure showed us there actually are pockets and that drugs could potentially be targeted to those pockets,” Aguirre adds.
Curious about the effect of mutations in SHOC2 amino acids, the team also performed extensive mutation studies of SHOC to understand the impact of all possible single amino acid mutations on SHOC2 function. They generated data that potentially can be used to understand the role of SHOC2 in other diseases, including Noonan-like syndrome, which causes distinctive facial features and other symptoms related to development.
A Team Effort
Aguirre is quick to point out that these insights into SHOC2 were only made possible through the collaborative efforts of many different experts from varying disciplines. “No one team could have done this alone,” Aguirre says. “We’re all very excited about developing drugs for this complex. The RAS research field in general is firing on all cylinders right now, and I think everyone’s hard work is going to lead to important benefits for patients.”