New NCCN Guidelines Stress Genetic Testing For All Pancreatic Cancer Patients

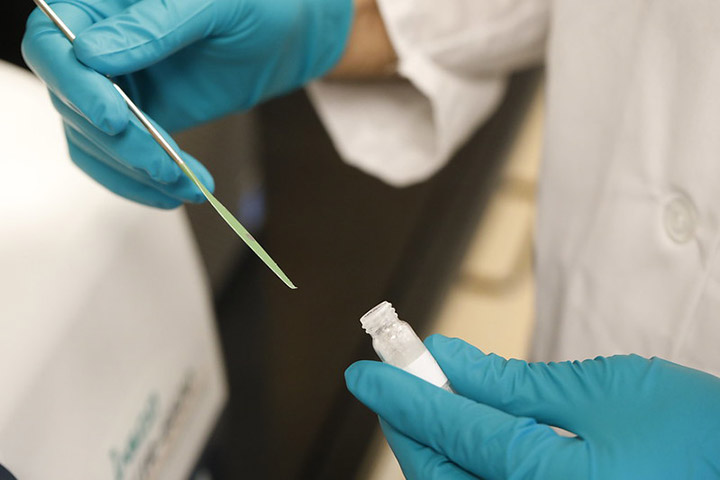
Courtesy of Dana-Farber Cancer Institute.
If you or someone you love has been diagnosed with pancreatic cancer, the message is clear: all pancreatic cancer patients should undergo genetic testing for inherited genetic mutations, regardless of family history.
That’s according to new guidelines established by the National Comprehensive Cancer Network (NCCN), a group of 27 expert cancer centers throughout the U.S. that provides recommendations called Clinical Practice Guidelines for the treatment of some 30 different cancer types. Under these new recommendations, pancreatic cancer patients should receive genetic testing for more than just the well-known BRCA1 and BRCA2 mutations, which are linked to ovarian and breast cancer, as well as pancreas and other cancers.
“Although there have been incredible leaps in the entire field of genetics, getting everyone on board with genetic testing isn’t the same thing as getting everyone on board with trying new drugs, which is a lot easier,” says gastrointestinal cancer genetics and prevention expert Dr. Sapna Syngal. “But solid steps have been made in pancreatic cancer genetics and the data have accumulated, we believe overwhelmingly, to show that every patient with pancreatic cancer—regardless of their family history—should get germline genetic analysis,” says Syngal, who serves as Director of Research, Center for Cancer Genetics and Prevention and Director, Gastrointestinal Cancer Genetics and Prevention programs at Dana-Farber Cancer Institute in Boston, Massachusetts.
Germline Mutations Are an Important Predictor
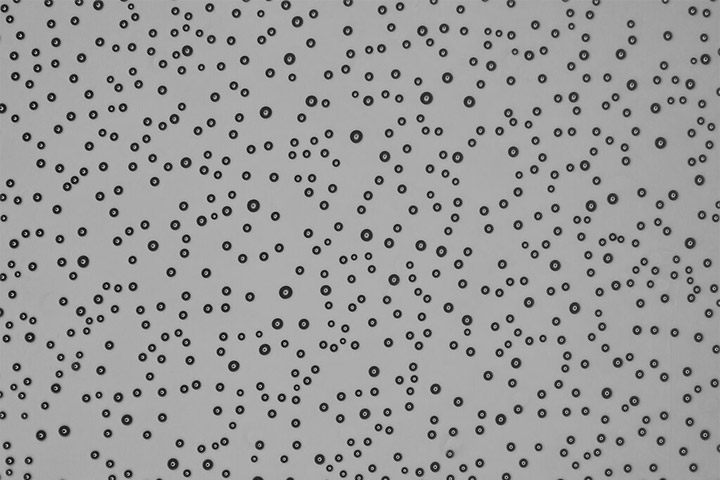
Somatic genetic mutations are random, and happen during a person’s lifetime. A germline mutation is an inherited mutation. That means a person is born with it. New research has shown just how important these germline mutations may be in pancreatic cancer development.
For example, a study published earlier this year in JAMA (Journal of the American Medical Association) showed that six genes contain mutations that may be passed down in families and substantially increase a person’s risk for pancreatic cancer. The genes include not only BRCA1 and BRCA2 but also CDKN2A, TP53, MLH1 and ATM. These genetic mutations were identified in 5.5 percent of all pancreatic cancer patients, including 5.2 percent of cancer patients without a family history of pancreatic cancer. This finding led the Mayo Clinic research team to recommend genetic testing for all pancreatic cancer patients as the new standard of care.
Genetic Testing for All
Prior to these new recommendations, an individual with pancreatic cancer met testing criteria only if they were of Ashkenazi ancestry or had family history of Hereditary Breast and Ovarian Cancer Syndrome (HBOC) cancers, which are most commonly caused by mutations in the BRCA1 and 2 genes, says Syngal, who along with Dana-Farber research scientist C. Sloane Furniss, Ph.D., wrote a JAMA editorial in support of the Mayo Clinic study recommendations.
However, the above groups combined account for only about 10 percent of pancreatic cancer patients. Although it’s tough to put a number on how many patients may have been affected, what is clear is that some patients fell through the cracks. “There were a lot of pancreatic cancer patients being missed in terms of genetic testing simply because they didn’t fit into the recommendations,” says Syngal. Now, after testing, all patients will have a chance to benefit from potentially helpful targeted, more personalized, treatments. For example, the presence of BRCA1 or BRCA2 mutations in a tumor has been found to predict response to certain therapies such as PARP inhibitors and platinum-based drugs.
A patient’s family members may benefit too, adds Dr. Syngal, since family members of a pancreatic cancer patient with a germline mutation might consider getting tested as well; family members may want to meet with a genetic counselor and learn about potential eligibility for pancreatic cancer and other cancer screening and prevention programs. It’s also important to know that having a germline mutation does not mean that you will develop pancreatic cancer, she says. Rather, it means that you are at greater risk.
What Should Patients—and their Families—Do
The most important thing is to be your own advocate and “talk to your doctor, because if you have pancreatic cancer your tumor should absolutely get tested,” Syngal emphasizes. Although NCCN guidelines are a kind of “gold standard” for insurance coverage, there is sometimes a lag between new guideline recommendations and coverage. “I think most doctors who treat pancreatic cancer patients are on board with this because of the data and because this presents a very exciting opportunity to help more people,” she adds. “The genetics are a piece of the puzzle that can help answer questions as to why this happened. We can potentially recommend targeted treatments to patients, and those treatments are getting better all the time—and we can help family members. This is a big step forward.”