Hope and a Chance to Fight
- Diagnosis at stage Ib
- A Whipple procedure right after diagnosis
- Chemotherapy as part of a clinical trial
- Five years later, scans remain clean
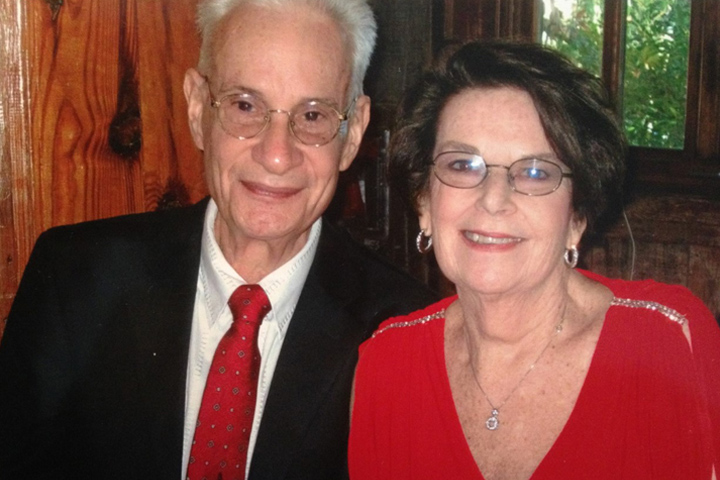
On February 13, 2013, my husband Irwin, 67, was diagnosed with pancreatic cancer. The bottom dropped from our world.
The previous day Irwin had passed out at school, where he had been teaching. He’s diabetic, so he assumed it was caused by low blood sugar. That night he experienced unbearable pain in his side and lower back. I wanted him to go to the ER at the hospital across the street from where we live in New York City, but he insisted that he would visit our primary care physician, Dr. Alan Kadet, at 8 a.m. the next morning. Dr. Kadet saw Irwin immediately. The doctor felt Irwin’s abdomen, which caused him to jump off the examining table. Dr. Kadet insisted that Irwin go to the ER at Roosevelt Hospital (now Mount Sinai West). Dr. Kadet called ahead so they were expecting us.
We were rushed in and the doctors immediately ordered blood tests and a CT scan of his abdomen. Three hours later I was called to the phone at the nurses’ station, and Dr. Kadet told me Irwin had pancreatic cancer. I can still feel the horror now four years later. I had to tell Irwin this devastating news. We both cried and felt totally lost, confused, and frightened. What were we to do? We knew nothing about this cancer.
Treatment Starts with Surgery
They moved Irwin to a room and we met with Dr. Barbara Wexler, who said that there was a doctor at this hospital who could perform a Whipple. They medicated Irwin so that he could sleep. The next morning, Dr. Fadi Attiyeh walked into Irwin’s room and said that he had reviewed the scans and that he would perform the Whipple. We looked at this man in amazement. He said the tumor was stage Ib and small (good), in the head of the pancreas (better), and that Irwin could be operated on within the week (OMG). So we had a surgery date within 18 hours of being diagnosed. A miracle.
The Whipple is a seven-hour operation. If it was successful it could help save his life. Dr. Attiyeh said we could do this and Irwin would be fine! Irwin had the surgery at the end of February. He withstood the pain thanks to the massive doses of medication. BTW when Dr. Attiyeh said Irwin would be “fine,” little did we know what that would mean to us.
A Clinical Trial to Wipe Out any Traces of Cancer
After recovering from surgery, Dr. Attiyeh told us there was a suspicious lymph node and Irwin would need a chemotherapy protocol. We met with Dr. Kenneth Yu at Memorial Sloan Kettering, who suggested a single drug, Gemzar. We got a second opinion with Dr. Robert L. Fine, at The Pancreas Center at Columbia Presbyterian Hospital. He was in charge of an experimental clinical trial. Irwin would receive an IV of Gemzar and Taxotere one day a week for two weeks, while taking pills of Xeloda every day for 14 days, then a week with no chemo to allow his body to rest. The program would run six months.
Irwin had no side effects for the first week, but then the side effects came on with a vengeance. Nausea, diarrhea, and weakness were typical. Irwin had metal mouth and no appetite. The only food he craved was pizza with strawberry preserves. His weight dropped to 120 lbs. from 135, and it was difficult to maintain even that weight. He became constipated, anemic (requiring several blood transfusions), developed black hairy tongue, shingles, chemo brain, and depression.
Despite all this Irwin followed the instructions from Dr. Fine and Dawn Tsushima, his nurse practitioner, to the letter. He wanted to be their best patient. Irwin wanted his survival to be a testament to Dr. Fine’s experimental trials. Dr. Fine’s trial was financed from a grant, but all of our expenses were covered from our employment health care policy, which was needed.
Thankful to Have Access to Top Care
Through all of this we always tried to stay positive and thankful. I kept a daily journal, which I later turned into a book, Lucky Journey: Surviving Pancreatic Cancer, from a caregiver’s point of view. It was cathartic to put my feelings on paper and then move on. New York City played a major role in his recovery. Having access to the top hospitals and surgeons, and the newest technologies, all were in his favor. The hospital where Irwin had his surgery was located across the street from where we lived; he received chemo a short 15-minute subway ride away from home, which was a gift.
Irwin had chest CT scans and MRIs of his abdomen and pelvis every three months for two years, then every six months for a year. Now he has scans once a year.
We know that pancreatic cancer patients don’t have good survival odds, perhaps 15 percent, but someone has to be in that 15 percent. We continue to believe. We participate in the Columbia Presbyterian Hospital Pancreatic Support Group, which meets the third Tuesday of each month. It gives us an opportunity to help other pancreatic patients and their families.
The most important thing is that Irwin is still alive and well almost five years later. Hope and the doctors gave us the chance to fight this dreaded disease.
Ten years after his pancreatic cancer diagnosis, Irwin passed away from unrelated causes. We offer our deepest sympathy to his family.





