Tailoring My Treatment to My Tumor Genetics

- Surgery, then chemotherapy
- Tumor genetics determines which drugs to use
- Low slow dosing of chemotherapy
In April 2016, while on a trip to Connecticut, I struggled with a belly pain and nausea that kept me up all night.
I had been having belly pain on and off for at least a year but this was different, more acute. When I arrived at Greenwich Hospital, a CT scan revealed a partial bowel obstruction, no movement in my small intestine, and a tumor in my pancreas. My world turned upside down.
I was 71 years old, and a wife, mother of six, and grandmother to eight beautiful grandkids. I had a successful career as a college professor, teaching science as well as social justice, and was working on a book when this diagnosis hit.
Now I would have to put into practice what I had been helping others to navigate—a serious illness, one that scientific literature said would likely cost me my life. An internet search quickly showed me the grim statistics but my kids kept finding stories of survivors from websites like Let’s Win.
Treatment Starts With Surgery
In mid-April I had surgery at Yale Medical Center to remove most of my pancreas and my spleen. The pathology report revealed that I had stage IV metastatic pancreatic adenocarcinoma. According to all the oncologists at various institutions I interviewed, chemotherapy was necessary and soon. I could gain more time but not a cure.
My recovery from surgery was complicated. I required a second surgery, at Greenwich Hospital, for bowel obstruction. The surgeon found that the cancer had spread to my peritoneum, the lining of the abdominal cavity. When my husband asked the surgeon who repaired my bowel obstruction how long I would survive, he said, “Two months.” I learned this two weeks later, and it sent me into a spiral of despair that almost cost me my hold on what I call my life force. I was giving up; giving in to the cancer and the grim diagnosis.
While in Greenwich Hospital, Dr. Barry Boyd, a very kind oncologist, came in to talk to me. We hit it off and he became my treating oncologist. I liked his respect for science and his belief that “everyone is different—not everyone falls into the Bell curve. There are outliers. We just don’t hear about them. They are not usually in the research studies.” He had had many people survive pancreatic cancer over his career.
Chemotherapy Tailored to Match My Tumor Genetics
Dr. Boyd told me the key is treating people as unique and then tailoring treatment to meet their specific situation. Analysis of my tumor showed that I had two broken genes that are significant for pancreatic cancer. I already knew that I am BRCA1 positive. But I also have a KRAS gene break. I learned that this gene is responsible for at least as much as 90% of pancreatic cancer!
After much soul-searching I agreed to six months of chemotherapy. I met Dr. Allyson Ocean at Weill Cornell and considered doing treatment with her. However, I wanted to continue with Dr. Boyd and to stay closer to my children’s homes in Connecticut as I was very weak after the two surgeries. Dr. Ocean, a colleague of hers in Los Angeles, Dr. William Isacoff, and Dr. Boyd ended up collaborating. They came up with a tailored cocktail for me that was not the usual standard treatment for this cancer. It was low, slow doses of 5-FU, cisplatin, and mitomycin-C. I was on a pump two weeks out of four, for six months.
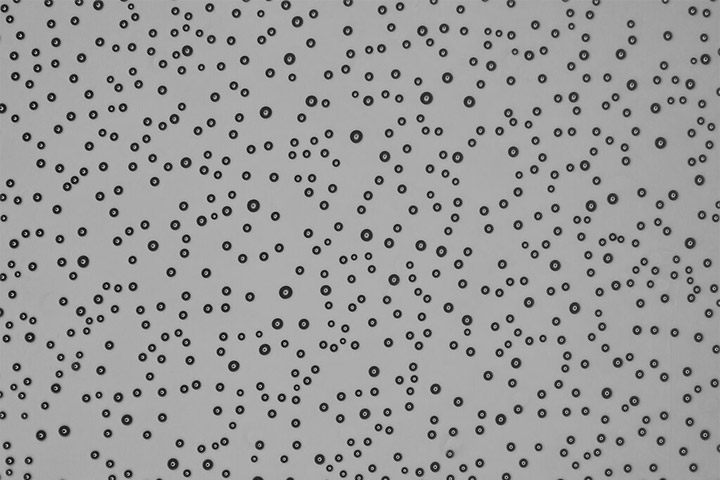
Some important research has shown that high doses of intravenous vitamin C can prevent replication of the pancreatic cancer cells. So I also sought intravenous (IV) vitamin C on the two weeks I was off the pump. I had 12 infusions in all in tandem with the chemotherapy. I also sought out alternative medicines and complementary treatments such as acupuncture on my own, though I told all my collaborating physicians about them.
I would not be doing as well as I am right now if it were not for my family who researched treatments, talked with doctors, took me and my husband into their homes (I have not yet returned home to California); doctor friends who also stayed with me during and after surgeries; my spiritual community at home who contributed prayers, stories, accompaniment, and financial support.
Disease Free!
Almost a year after my diagnosis, all my tumor markers have normalized. I was scheduled to begin an IV vitamin C trial that Dr. Ocean is facilitating at Weill Cornell, but she confirmed what Dr. Boyd had told me previously: There is no evidence of disease—I don’t fit the trial.
But I know this cancer’s reputation. It can sneak back. So, I am taking the IV vitamin C on my own. I am grateful to these oncologists for their willingness to think and treat outside the box—to tailor treatment to the individual using the best science available at the time and to collaborate in my treatment!
Sharon tells her story in “I’m Going to Live Every Day.”
Read more about the vitamin C research at Weill Cornell in the article “Testing Vitamin C as a Cancer Killer.”