Chemotherapy Makes Tumor Removal Possible

- Treatment with Xeloda
- More chemotherapy with gemcitabine and 5-FU
- Whipple surgery to remove the tumor
In December of 2006 at the age of 56 I became aware of a slight pressure in my side.
I decided to follow up with my doctor. She recommended a CT scan to see if I had gallstones or appendicitis. The pressure subsided and I considered ignoring her advice. Fortunately, I went ahead with the CT scan. To my surprise, my doctor called the next day to tell me I had what looked like a tumor on my pancreas. She scheduled me for an endoscopic biopsy to confirm the diagnosis.
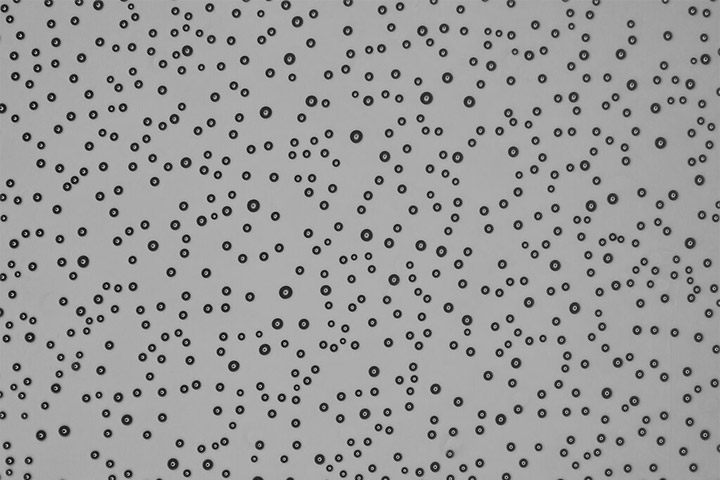
On January 31, 2007 after an endoscopic biopsy at Hoag Hospital in Newport Beach, California, I was advised that I had pancreatic cancer. Within 24 hours I was referred to Dr. Howard Reber of UCLA for surgery on the tumor that was on my pancreas. At my initial meeting with Dr. Reber, I was told he was unable to perform surgery at that time because the tumor had invaded an artery. Twenty minutes later I had a meeting with Dr. William Isacoff, an oncologist at UCLA. Dr. Isacoff immediately started me on a pill form of chemotherapy called Xeloda, which I took for a short time.
Chemotherapy Begins
Several days later my treatments began. I received gemcitabine and 5-FU. I received chemotherapy intravenously for approximately two hours a day, twice a week, every other week. The treatment made me feel very tired, but other than the first day of treatments, I was not really ill. Typically, I was not able to function at full strength for the first few days after chemo, but became stronger with each passing day. Once I began to recognize the pattern the treatments became much more bearable and I was able to schedule my life around them. As the months went by and my red blood cell count dropped, I became less tolerant of the chemotherapy. Sometimes I couldn’t even receive my treatment and I had to get a blood transfusion instead. The transfusions became a welcome occurrence because I felt so much better after them.
Emotionally I went through a lot of ups and downs. I had so much support from family and friends, who came in from out of town to help. I also felt that I had pared down my life to ‘what really mattered.’ I stopped worrying about the many things that seemed so important before. But because of treatment and recovery from treatment, any time I had available to me was essentially cut in half.
I did very little Internet research about pancreatic cancer, because I didn’t want to know about any statistics or ‘my odds.’ I am convinced attitude plays a big part in getting better. I think it would have been much harder to maintain a positive attitude knowing the grim statistics of pancreatic cancer. For me, getting better and returning to my regular life was the only option I ever considered.
As the months wore on, I began having a harder and harder time with the chemo. It was summer, it was hot, I had gained about 20 pounds and nothing fit. I always seemed to be sweating and out of breath. I think what carried me through these months was the fact that I almost always had good news when I went to the oncologist’s office. My numbers were always dropping. My CT scans showed the tumor was shrinking. Almost every time I went I gleaned some piece of information that made me feel I was getting better.
Surgery Becomes Possible
In August 2007, after seven months of chemo I had another CT scan and an endoscopic ultrasound to see if it was time for Whipple surgery. The results looked good for surgery and I went back to Dr. Reber. I was expecting a long wait but my surgery was scheduled for September 17, a good omen for me as it was my late father’s birthday. In spite of some recovery complications my surgery was deemed to be a great success. My pathology afterwards showed me to be cancer-free. Every day I felt stronger and better.
It has been 10 years. I go in for a checkup about every six months. I do not have any complications from the cancer or the surgery. I do not take any medications relating to pancreatic cancer. I truly feel I owe all that I have gained to Dr. Isacoff and Dr. Reber. I will always be thankful that I was directed there and I continue to be in touch with other cancer patients.
Watch Anne’s story in her Video “Don’t Believe the Odds.“